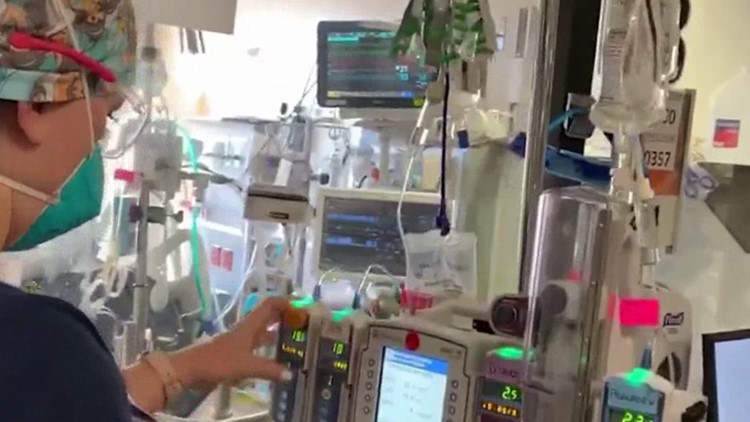
JACKSONVILLE, Fla — It is a critical piece of life-saving equipment many probably never heard of unless their loved one has needed it. During the pandemic some of the sickest COVID patients with severe lung disease have been placed on an ECMO machine.
"What it stands for is extracorporeal membrane oxygenation. What that confusing term means is outside of the body gas exchange device or an artificial lung. Why it's useful in the setting of ECMO is many of our ECMO patients have severe lung disease, pneumonia, and ultimately, that's a source of death for most patients," Dr. Steven Keller explained. "For patients who are not able to be supported on traditional ventilators, it's possible to support patients for a variable period of time using this experimental therapy called ECMO."
Dr. Steven Keller, an instructor at Harvard Medical School, is Medical Director of the ECMO mechanical support service at Brigham and Women's Hospital in Boston. He works with patients on ECMO in the Intensive Care Unit.
ECMO is reserved for the sickest patients who are not able to use the ventilator.
It is a highly invasive therapy that carries its own risks, and requires a great deal of expertise to perform safely. While hospitals like Mayo Clinic and UF Health in Jacksonville have ECMO machines, they are in high demand right now. The Extracorporeal Life Support Organization (ELSO) has map showing ECMO availability.
Dr. Keller says there are two parts to ECMO, the machine itself and the expertise in managing it.
"Certainly in the setting of a national pandemic, I would certainly say we're at capacity," Keller explained. "Every aspect of it, machine capability, our physicians, nurses ECMO specialist capacity, all of those are at capacity. It varies region by region, of course."
One of the big challenges he said is that the patients who require ECMO oftentimes are so sick, that they are not able to travel to an ECMO center.
"One of the areas of building capacity is travel ECMO teams. That is something that is relatively new in this field and expanding, but the ability of teams with capacity to put a patient on ECMO, to travel to the patient and initiate ECMO support," Keller explained. "That's an area that is still very much growing and developing in the country, but I would say, as a country, we're not there yet, and so there's a lot of work to be done."
Keller said those that benefit most from ECMO are patients who were younger and healthy before they became ill. Part of this is some of these patients see the sharpest decline in the health.
"If you get really sick really fast, you're more likely to get benefit from ECMO versus if you've gotten sick over a slower period of time, have developed more extensive lung injury before you get supported with the device," Keller said.
Patients can stay on ECMO for months, and studies show it's helping save lives.
"We suspect that the vast majority of those who wouldn't have been put on ECMO would likely have passed," Dr. Keller said. "So if we're getting a 50% survival, we would compare that against I would estimate less than 5% survival. So that is a market increase. We think we're saving a lot of lives by doing this."